Knowledge
Targeting Spine Behavior In Your Programming
Articles, Rehab, mobility & injury prevention

Behavior Of The Spine
The spine is a dynamic system, and as with any system, it requires stability to efficiently carry out its function. Function and stability are often ill-defined, so let’s discuss these first. A blanket definition for a function is “an activity or purpose natural to or intended for a person, thing, system”, while stability can be defined as “the ability to resist to change and/or return to a position of equilibrium following perturbation”.
A system is functional if it is able to perform the activity for which it was intended, and stable if it can resist change or recover completely following disturbance.
The human body is a multi-link structure, involving segments connected to one another not only structurally, but via a complex soft-tissue system: the kinetic chain. The spine is multisegmental in nature and as such, stable behavior of the spine is crucial to allow movement and bear loads.
Assessing The Spine
I have often had trainers tell me that one aspect where they lack clear direction is client assessment. I think the assessment is an opportunity to utilize a problem-solving approach, but it’s also an ongoing process. No one protocol will be useful for all your clients, and typically, one stand-alone assessment will not tell you everything you need to know. As Christian Thibaudeau says, “a good coach is not a program writer, he is a problem solver”.
I do think that we need some direction in how to approach assessment and how to problem-solve at every session. For some time now, there has been some debate around posture, specifically around the value in assessing it and whether or not we can truly have an impact on it through training.
There are many aspects to managing posture beyond the scope of this article. From a training perspective, I have always proposed that you need to be aware of posture (and its consequences) so that you can efficiently manage it in some aspect of your programming.
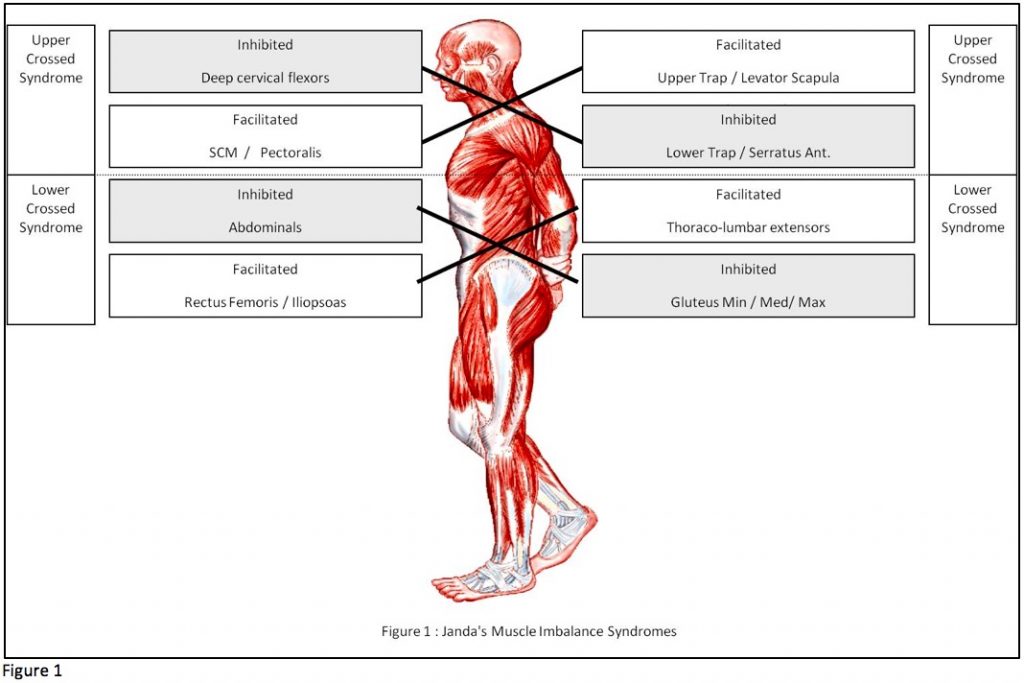
Dr. Vladimir Janda was highly influential in the importance of thinking in terms of muscle function rather than strength (Figure 1). His upper crossed, lower crossed and layer syndromes allow us to think in terms of inhibition and facilitation as a way to identify systematic and predictable muscle imbalance: inhibited muscles are unable to achieve an appropriate level of tone to execute a movement, while facilitated muscles are pre-disposed to fire first, which only further inhibits the former.
Although this may sound like a tightness or weakness problem, it’s actually a command problem: if we want successful activation of one muscle, we need deactivation of an overactive (facilitated) muscle, but this can’t be achieved with simply isolated strengthening and static stretching.
Even the evolution of bipedalism that occurred over billions of years was accompanied by a large number of skeletal changes as an adaptation to repetitive behavior in the upright position.
We didn’t come to stand more upright because the apes started stretching their pecs against the cave door and rowing tree trunks. It’s largely about what you repetitively do.
How Do I Manage This?
Posture assessment (Janda’s approach) gives you a global view of muscle imbalance and predictable motor command problems. It also allows you to predict the behavior of the spine. For example, in the upper crossed syndrome, you will observe a forward head (cervical hyperextension) and rounded upper back (excessive thoracic kyphosis). This is the behavior you will want to target.
Because our brain is wired to compensate around mobility first, I like to apply the Joint-by-Joint Approach (Cook & Boyle) to manage spine behavior. As Gray Cook says, you want to add length before you add strength. Note that muscles that have been reflexively inhibited by tight antagonists often recover after addressing the tightness, but how you address the tightness is of utmost importance.
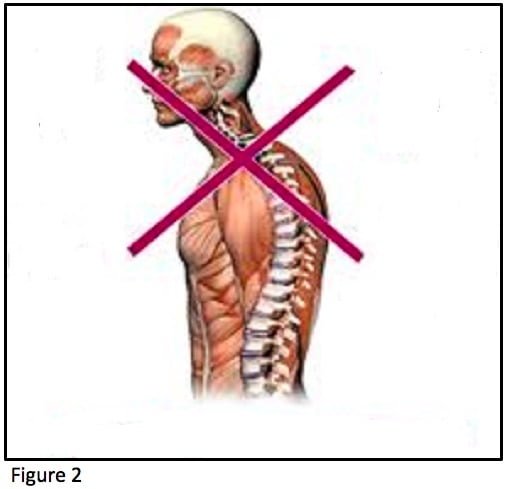
The cervical and thoracic portions of the spine were designed for mobility. The upper crossed syndrome essentially “locks” them into one position, resulting in the loss of this intended mobility, and this is compensated for at other levels by giving up a degree of stability.
The classic example is the loss of scapula-thoracic stability to make up for lack of thoracic mobility. The faulty position of the scapula then compromises the capacity for proper joint centration, it’s a vicious cycle. Using a mobility first approach, you will target cervical and thoracic mobility predominantly and continuously.
How Does It Look?
To put this all into more practical terms, here are the many ways I might manage upper-crossed syndrome in my overall planning:
- Include cervical mobility in all sessions/warm-up (teeth together chin-to-chest)
- Include thoracic mobility in extension in all sessions/warm-up
- Include dynamic scapular stability exercises in all sessions/warm-up (typically preceded by mobility exercises)
- Include PNF strengthening patterns for the upper extremity and PNF stretching techniques for the pecs and upper traps all sessions/warm-ups
- Use mobility exercises as a rehab primer prior to the main exercise (eg. Chin-to-chest 10 reps prior to a set of overhead presses or thoracic extension 10 reps prior to a set of squats)
- Use dynamic stability exercises as a rehab primer prior to the main exercise (eg. Scap/serratus press for 5 controlled reps prior to a set of bench presses or forearm wall slides for 5 controlled reps prior to a set of overhead squats)
- Use a push/pull training system rather than straight sets of pushing/pulling alone
This is just a simple example. You can apply this all the way up (or down) the kinetic chain, and it will be applied based on the degree of need for correction (more to come on that, so stay tuned!). The idea is to direct the spine towards the behavior you want in the long-term (or manage the inappropriate behavior, depending on how you want to look at it), as well as how you want it to behave for that session.
*Remember the following:
- For the mobility exercises, you need to move actively beyond the range of motion that is easily accessible to you.
- Your primers need to follow a low-threshold strategy: they should be controlled, non-fatiguing, and low-speed.
– MLD